If you’ve been experiencing unexplained tooth pain that doesn’t seem to go away, you may be wondering if you might need a root canal procedure. Root canal infections can lead to severe pain, abscesses, and even tooth loss. Identifying the signs of a root canal issue is crucial. If you are exhibiting the symptoms of a root canal infection, you should seek proper dental care urgently.
Table of Contents
ToggleWhat Is A Root Canal?
A root canal infection is a condition where the dental pulp inside the tooth root becomes infected or inflamed. The pulp contains nerves, blood vessels, and connective tissues that help in tooth development. When bacteria enter the tooth through a cavity, crack, or injury, it can cause an infection in the pulp. A root canal procedure, also known as endodontic treatment, is a dental procedure that is performed to remove the infected or inflamed pulp from the tooth.
Causes Of An Infection In The Tooth Pulp
There are several causes of an infection in the tooth root, including severe tooth decay that progresses deeper into the tooth, reaching the root canal.
A traumatic injury to the tooth, such as a fracture or a hard blow, can damage the blood vessels and nerves inside the tooth, which allows bacteria to enter the root canal. Cracked or broken teeth from other causes can expose the inner layers of the tooth to bacteria, too.
Advanced gum disease, also known as periodontitis, can cause the gum tissues to recede and create pockets around the tooth. Bacteria can then accumulate in these pockets, leading to infection of the tooth root.

Individuals with a weakened immune system, either due to certain medical conditions or certain medications, are more susceptible to tooth root infections.
Timely dental care, regular check-ups, and good oral hygiene can help prevent tooth root infections or detect one early.
Root Canal Symptoms
There are seven symptoms that are common indicators of an infected tooth pulp; these indicate you may need a root canal treatment. Individual symptoms can vary, so diagnosis by a dentist or endodontist is required before knowing definitively whether a root canal is necessary.
Severe Tooth Pain
Persistent and intense pain in a specific tooth is often a sign that the nerve tissue inside the tooth is infected or damaged.
Sensitivity to Hot or Cold
Increased sensitivity to hot or cold temperatures, especially when the sensation lingers even after the source of heat or cold has been removed, could indicate the need for a root canal.
Swollen or Tender Gums
Inflammation or tenderness in the gums around a particular tooth may indicate an infection that requires root canal treatment.
Discoloration of the Tooth
A tooth that is darkened or discoloured compared to the surrounding teeth may be a sign of internal damage or decay.
Pimple Or Abscess
A pimple-like bump or a small pus-filled sac on the gums near a tooth can be a sign of infection. Accompanied by pain or discomfort in the area, it indicates the need for a root canal.
Pain When Biting Or Applying Pressure
If you feel pain or discomfort when chewing or applying pressure on a particular tooth, it can be an indication of a damaged nerve and the need for a root canal.
Loose Tooth
A tooth that becomes loose or feels unstable might require root canal treatment to address the underlying damage or infection.
How Does Endodontic Treatment Save the Tooth?
Endodontic treatment, also known as a root canal treatment, saves the tooth by removing the infected or damaged pulp from the tooth’s internal chamber and canals in the root. This prevents the infection from spreading further and causing more damage. By removing the infection, the tooth does not need to be extracted to stop the infection. Simply taking antibiotics is unable to effectively treat a root canal infection, so this procedure is necessary.
Step-by-Step Endodontic Procedure
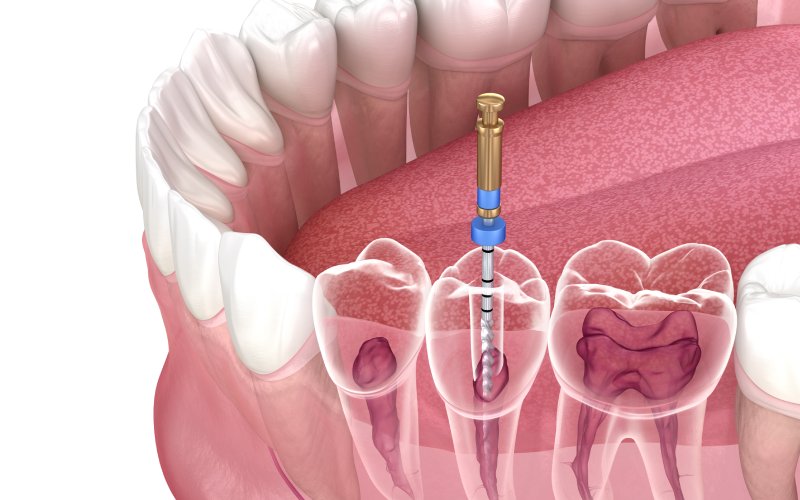
The dentist administers local anesthesia to numb the area around the affected tooth, and then creates a small access hole in the tooth’s crown to reach the pulp chamber. Dental tools are used to carefully remove the infected or damaged pulp from the pulp chamber and root canals.
Next, your dentist thoroughly cleans and shapes the canals using tiny files to remove any remaining pulp or bacteria and help prevent reinfection. Antimicrobial solutions are used to rinse and disinfect the canals further, killing any remaining bacteria.
After cleaning and disinfecting, the canals are filled with a biocompatible material called gutta-percha, which helps seal the canals and prevent recontamination.
In some cases, a second root canal treatment may be necessary to ensure the canal is completely cleaned and treated, so a temporary filling is used until that second visit.
A permanent restoration like a dental crown is often placed on the tooth to protect and strengthen the tooth. By removing the infected pulp and sealing the canals, endodontic treatment eliminates the source of infection and prevents further damage.
Will I Feel Pain During Or After The Root Canal Therapy?
Your tooth may feel sensitive during and after a root canal procedure. However, your dentist will use local anesthesia to numb the area and minimize discomfort during the procedure. Afterward, any soreness or sensitivity in the treated area can usually be alleviated with over-the-counter pain medication.
On the other hand, not treating a root canal infection would result in significant pain until it is treated,
Does Root Canal Therapy Kill The Tooth?
A root canal treatment involves removing the infected or damaged pulp from the tooth’s root canal and sealing it to prevent further infection. While the procedure does remove tissue from the tooth, it does not kill the tooth. Dental pulp nurtures teeth during development but becomes non-essential once teeth mature. The outer structure of the tooth, including the enamel and dentin, can continue to provide functional support to the tooth without live pulp. However, over time, the tooth may become more prone to breakage, which is why a crown is often placed to strengthen it.
Do You Need A Root Canal Treatment? What Happens If You Aren’t Treated?
If you don’t get a root canal when it is recommended or necessary, the consequences can vary depending on the specific condition of the affected tooth.
Spreading Infection
If the tooth is infected due to deep tooth decay or trauma, the infection can continue to progress and spread to the surrounding tissues, including the jawbone, gums, and other teeth. This can lead to a painful dental abscess or a more severe infection known as cellulitis.
Tooth Loss
Without a root canal, the infection can cause irreversible damage to the tooth and its supporting structures. In such cases, extraction of the tooth might be the only remaining option. Losing a natural tooth can lead to further complications, such as difficulty chewing and speaking, jawbone loss, shifting of adjacent teeth, and aesthetic concerns.
Chronic Pain
A tooth in need of a root canal is often very painful due to the infection reaching the nerves and root canal system. Ignoring the treatment can result in ongoing or worsening pain.
Health Risks
While rare, severe dental infections have been linked to systemic conditions such as endocarditis (heart valve infection) or infections in other parts of the body.
Financial Implications
Delaying or avoiding a necessary root canal can lead to additional dental treatments becoming necessary. This can result in higher costs in the long run, as well as potential tooth replacement options like dental implants or bridges.
See Your Dentist
If you are experiencing any of the common signs you need a root canal, see your dentist as soon as possible for diagnosis and treatment. Gateshead Dental provides root canal treatments in our office. We’ll answer all of your questions and address any concerns you have. Get relief from your pain, and don’t suffer longer than necessary.
He’s completed a number of additional courses to best serve his patients and be able to educate them too. No matter your age or dental condition Dr. Sims can assist you in a professional manner and loves answering any of your questions or concerns.
- How to Care for Dental Implants - April 26, 2024
- Is It Safe to Have Dental Work Done During Pregnancy? - February 28, 2024
- How Does A Dental Bridge Work? - January 17, 2024
